
Dr. Swapan Kumar De
Senior Most Interventional Cardiologist at
Apollo Multispeciality Hospital Kolkata.
MD, DM (Cardiology)
Angioplasty Doctor in Kolkata, India

Percutaneous coronary intervention (PCI), commonly known as coronary angioplasty or simply angioplasty, is one therapeutic procedure used to treat the stenotic (narrowed) coronary arteries of the heart found in coronary heart disease. These stenotic segments are due to the build up of cholesterol-laden plaques that form due to atherosclerosis. PCI is usually performed by an interventional cardiologist, though was developed and originally performed by interventional radiologists.
Coronary artery bypass grafting (CABG), which bypasses stenotic arteries by grafting vessels from elsewhere in the body, is an alternative treatment. Most studies have found that CABG is better than PCI for reducing death and myocardial infarction. However, PCI does improve quality of life. PCI has proven to be as effective and less costly than CABG in patients with medically refractory myocardial ischemia.
The term balloon angioplasty is commonly used to describe percutaneous coronary intervention, which describes the inflation of a balloon within the coronary artery to crush the plaque into the walls of the artery. While balloon angioplasty is still done as a part of nearly all percutaneous coronary interventions, it is rarely the only procedure performed.
Other procedures that are done during a percutaneous coronary intervention include:

Sometimes a small mesh tube, or "stent", is introduced into the blood vessel or artery to prop it open using percutaneous methods. Angioplasty with stenting is a viable alternative to heart surgery for some forms of non-severe coronary artery disease. It has consistently been shown to reduce symptoms due to coronary artery disease and to reduce cardiac ischemia, but has not been shown in large trials to reduce mortality due to coronary artery disease, except in patients being treated for a heart attack acutely (also called primary angioplasty). In acute cases, there is a small but definite reduction of mortality with this form of treatment compared with medical therapy, which usually consists of the administration of thrombolytic ("clot busting") medication
The angioplasty procedure usually consists of most of the following steps and is performed by physicians, physician assistants, nurse practitioners, nurses, radiological technologists and cardiac invasive specialist; all of whom have extensive and specialized training in these types of procedures.

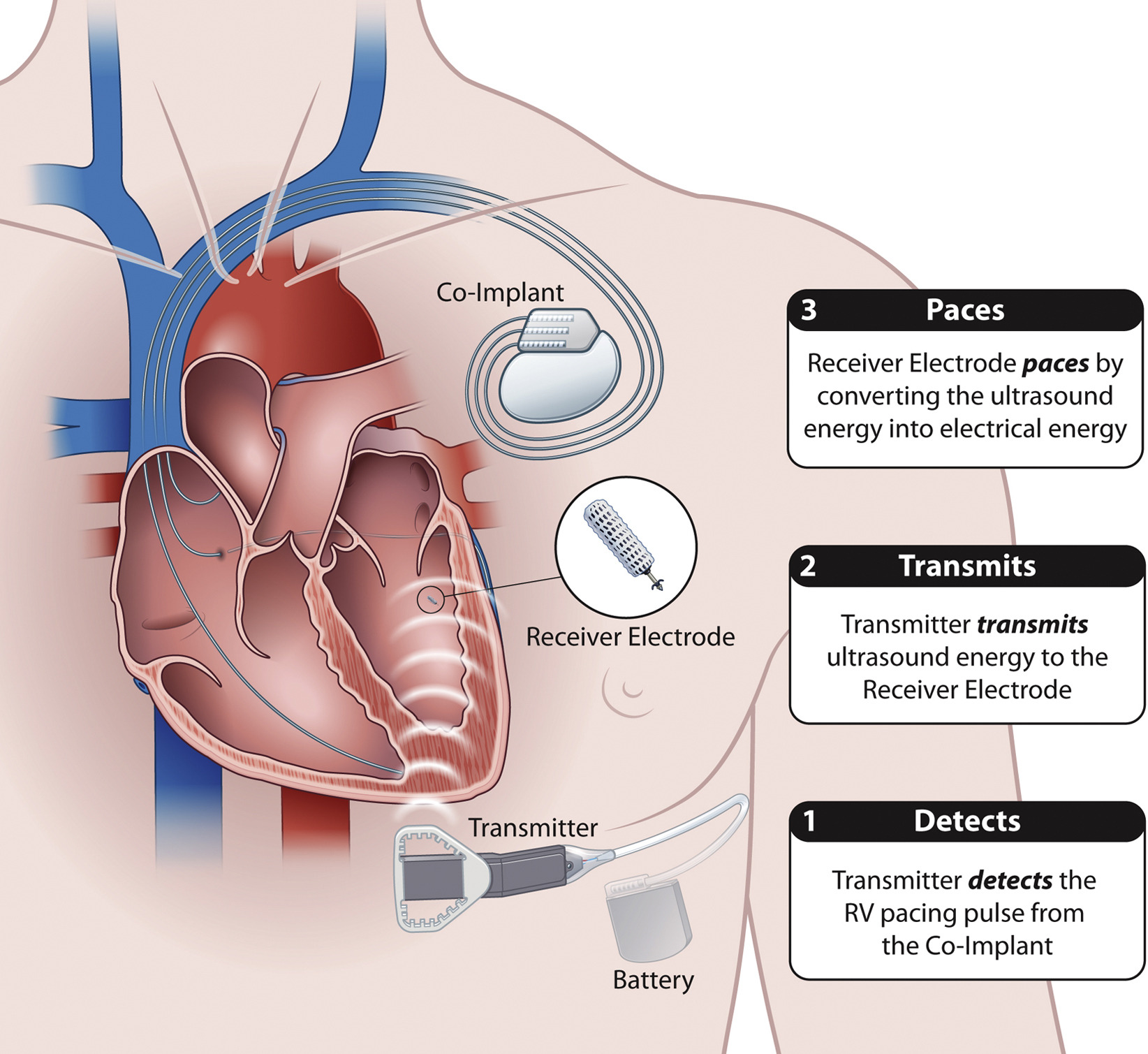
If someone has heart failure and have developed arrhythmia, he may be a candidate for cardiac resynchronization therapy (CRT).
Arrhythmias are irregular heart rhythms and can be caused by a variety of reasons, including age, heart damage, medications and genetics. In heart failure patients CRT, or biventricular pacing, is used to help improve the heart's rhythm and the symptoms associated with the arrhythmia.
The procedure involves implanting a half-dollar sized pacemaker, usually just below the collarbone. Three wires (leads) connected to the device monitor the heart rate to detect heart rate irregularities and emit tiny pulses of electricity to correct them. In effect, it is "resynchronizing" the heart.
Because CRT improves the heart's efficiency and increases blood flow, patients have reported alleviations of some heart failure symptoms - such as shortness of breath. Clinical studies also suggest decreases in hospitalization and morbidity as well as improvements in quality of life.
In general, CRT is for heart failure patients with moderate to severe symptoms and whose left and right heart chambers do not beat in unison. However, CRT is not effective for everyone and is not for those with mild heart failure symptoms, diastolic heart failure or who do not have issues with the chambers not beating together. It is also not suitable for patients who have not fully explored correcting the condition through medication therapies. To date, studies show CRT to be equally effective for both men and women.
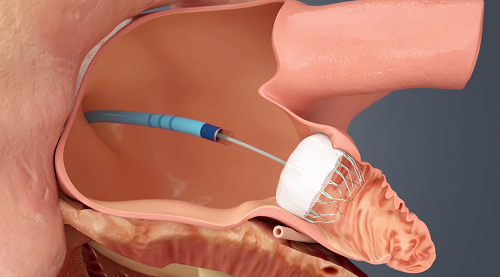
Left atrial appendage occlusion (LAAO), also referred to as left atrial appendage closure (LAAC), is a treatment strategy to reduce the risk of left atrial appendage blood clots from entering the bloodstream and causing a stroke in patients with non-valvular atrial fibrillation (AF).
In non-valvular AF, over 90% of stroke-causing clots that come from the heart are formed in the left atrial appendage.The most common treatment for AF stroke risk is treatment with blood-thinning medications, also called oral anticoagulants, which reduce the chance for blood clots to form. These medications are very effective in lowering the risk of stroke in AF patients. Most patients can safely take these medications for years (and even decades) without serious side effects.
However, some patients find that blood thinning medications can be difficult to tolerate or are risky. Because they prevent blood clots by thinning the blood, blood thinners can increase the risk of bleeding problems. In select patients, physicians determine that an alternative to blood thinners is needed to reduce AF stroke risk. Approximately 45% of patients who are eligible for warfarin are not being treated, due to tolerance or adherence issues. This applies particularly to the elderly, although studies have indicated that they can also benefit from anticoagulants.
Left atrial appendage closure is an implant-based alternative to blood thinners. Like blood thinning medications, an LAAC implant does not cure AF. A stroke can be due to factors not related to a clot traveling to the brain from the left atrium. Other causes of stroke can include high blood pressure and narrowing of the blood vessels to the brain. An LAAC implant will not prevent these other causes of stroke.
About Cardiologists : Cardiologists treat people with diseases or conditions of the heart and people who want to learn the risk factors for heart disease. A primary care doctor or family practice doctor can work with a cardiology specialist to diagnose, treat, and manage heart conditions and help people make heart-healthy lifestyle choices. Patients who are at risk for heart disease or have a history of heart symptoms may see a clinical cardiologist regularly. People with ongoing heart conditions, pacemakers, or frequent heart trouble are likely to see a cardiologist with a subspecialty.